VENOUS DISEASE / VEIN CLINIC
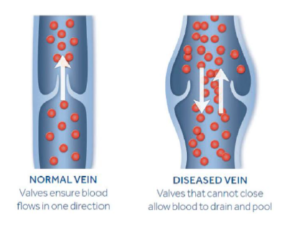
Venous disease occurs when the valves in the legs that regulate the one-way flow of blood in the veins become diseased and unable to function properly, leading to blood flow in both directions.
The most common causes of venous insufficiency are previous cases of blood clots and varicose veins. In some cases, weakness in the leg muscles that squeeze blood forward can also contribute to venous insufficiency.
Symptoms of Venous Disease include:
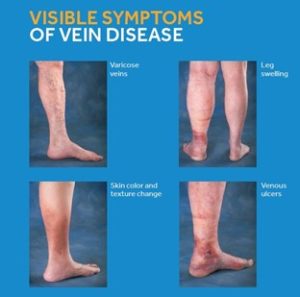
- Edema, or swelling, in the lower legs and ankles, especially after standing
- Itchy or flaky skin on the legs and feet
- Leg cramping or weakness
- New varicose veins or worsening of existing varicose veins
- Skin discolorations or leathery skin on the legs
- Tired, achy legs and feet, sometimes with burning or throbbing sensations
- Ulcers or wounds on the legs and ankles that have trouble healing
About 40% of all Americans have chronic venous insufficiency. Risk factors include:
- Swelling of a superficial vein (phlebitis)
- Family history of venous insufficiency
- Sitting or standing for long periods of time without moving
- Blood clots
- Varicose veins
- Obesity
- Pregnancy
- Smoking
- Cancer
- Muscle weakness, leg injury, or trauma
Spider veins (also called telangiectasias) are clusters of tiny blood vessels that develop close to the surface of the skin. They are often red, blue, or purple; and they have the appearance of a spiderweb. They are commonly found on the face and legs.
Varicose veins are not only cosmetic – they are swollen, twisted, painful veins that appear at the surface of the skin. Varicose veins are a result of a condition known as Venous Insufficiency or Venous Reflux. They occur most commonly in the feet and ankles, and, are a result of weakened or failed valves. The calf muscle helps move blood from the legs back into the heart. If the vein fails, blood cannot return to the heart and stays in the legs. Left untreated, this condition continues to get worse and can lead to serious complications and a blood clot.
A pulmonary embolism (PE) occurs when a blood clot that has formed in the veins breaks loose and travels through the bloodstream to the lungs, blocking blood flow to the lungs. A pulmonary embolism can cause sudden chest pain and shortness of breath. If a blood clot is large or there are many clots, a pulmonary embolism can cause death.
In early stages of vascular disease, conservative therapies provide good options for disease management. These include aggressive risk factor modification, smoking cessation, antiplatelet therapy and a walking program are essential. Compression stockings can also provide some relief of symptoms. These stockings apply steady pressure to help move the blood back to your heart. The steady pressure also lessens swelling in your lower legs and reduces the risk of getting a blood clot.
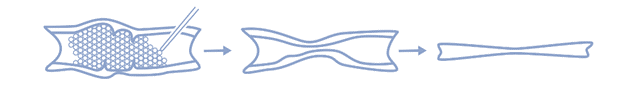
Sclerotherapy is the most common treatment for leg veins. Sclerotherapy causes the walls of the vein to stick together, so the blood cannot flow through it anymore. This improves circulation in the treated leg and reduces swelling. During sclerotherapy, your provider injects a chemical into the spider or varicose vein. (Different areas of the vein are injected). A compression stocking or wrapping is placed on the leg following the procedure. Patients can return to most activities or work the next day. Patients are recommended to walk daily while wearing the compression stocking after the procedure. Spider veins usually disappear in 3 to 6 weeks. Varicose veins take 3 to 4 months.
Radiofrequency Ablation (RFA) is a minimally invasive procedure that is used to treat varicose veins. During the RFA procedure, the provider will insert a radiofrequency catheter into the diseased vein. The provider will then guide the catheter through the vein, using an ultrasound to see inside the patient. Once the catheter is into position, RFA uses a thin laser fiber or radiofrequency catheter to produce heat to cauterize the damaged or weakened veins and collapse and close the varicose vein. As the body begins to recover from the procedure, patients can expect to see the treated veins shrink and fade away as blood flow is redirected towards healthier veins.
The VenaSeal system delivers a small amount of a specially formulated medical adhesive to seal — or close — the diseased vein, rerouting blood to nearby healthy veins, which provides symptom relief. VenaSeal does not require the use of tumescent anesthesia. As the body begins to recover from the procedure, patients can expect to see the treated veins shrink and fade away as blood flow is redirected towards healthier veins.

A small needle and hook are introduced into the vein after it is numb. The physician then snares the vein and removes it from the leg.
The inferior vena cava (IVC) carries blood from your lower body to your heart and lungs. It is the largest vein in your body. When blood clots form below the heart, they block normal blood flow and may cause swelling, redness, and pain in the area. If the clot(s) cannot be treated with blood thinners, a small device called an IVC filter may be placed in your inferior vena cava to prevent the clot(s) from moving through the blood into the lungs (resulting in a pulmonary embolism).
Your cardiologist will place the IVC filter in your inferior vena cava by going through a vein in your neck or groin. Your doctor will position the IVC filter in the vein using a fluoroscope (real-time x-rays).
